
Key Takeaways
- Your risk of developing cancer is affected by diet and lifestyle, genetic factors and age
- Screening tests are used to find cancer or cell abnormalities that might develop into cancer, in people who have no symptoms
- It’s important to attend screening tests so cancer may be caught early, and before it has spread
- The NHS offers three types of screening tests – cervical, breast and bowel
- It’s important to continue attending screening appointments for as long as you are eligible
Your risk of developing cancer can be affected by many things, including your diet, lifestyle, and genetic factors. Your risk for certain cancers can also vary simply with age. This is where screening comes in. Screening tests are used to find cancer or cell abnormalities that might develop into cancer, in people who have no symptoms. Regular screening gives you the best chance of finding cell abnormalities and cancer early. In the UK, the NHS offers three screening tests – cervical, breast and bowel. This article examines each of these in detail, including the age at which you’ll be invited for screening.
What’s your risk?
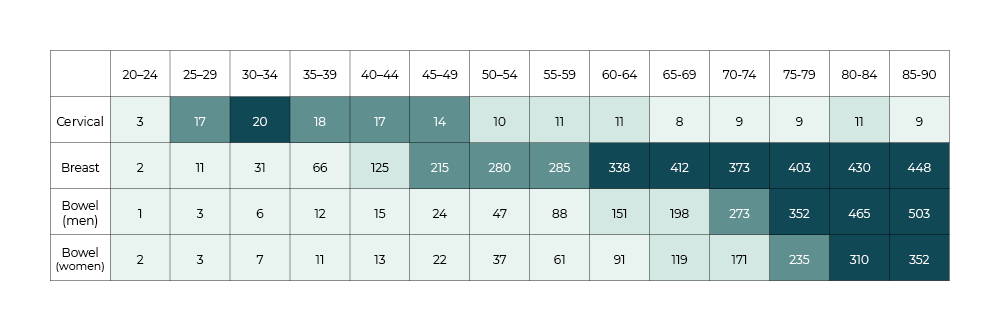
The chart below shows the incidence of cervical, breast and bowel cancer per 100,000 of the population. This will help to give you an idea of your level of risk based on your age, and therefore the importance of attending screenings. As you can see, your risk of cervical cancer peaks between the ages of 30 and 34, whereas your risk of developing breast or bowel cancer increases steadily as you get older.
How important is screening for those who have a family history of certain cancers?
Dr Vishakha Tripathi, Consultant genetic counsellor
When an individual is at an elevated risk for cancer, for example if they have a family history of the disease, access to regular evidence-based screening offers the opportunity for early detection and maximises options around treatment. If you have concerns about a genetic risk for a certain cancer, and there is either no screening programme for it or you haven’t yet been invited because of your age, you should have a conversation with a clinical expert, such as a genetic counsellor or clinical geneticist. This will help you to understand the evidence behind the screening options and the ages at which they’re available. It can also help you to understand other strategies to manage the risk that might be available to you. You can be referred to a genetic counsellor through your GP or a specialist hospital team.
When an individual is at an elevated risk for cancer, for example if they have a family history of the disease, access to regular evidence-based screening offers the opportunity for early detection and maximises options around treatment.
Dr Vishakha Tripathi, Consultant genetic counsellor
Cervical screening
About cervical cancer
Cervical cancer is cancer of the cervix – the opening from the top of the vagina to the womb. The main cause of cervical cancer is a virus called high-risk human papillomavirus (HPV), which can cause abnormal cell changes that may develop into cervical cancer. At the early stage, cervical cancer may not cause any symptoms and is usually found and treated because of cervical screening tests, which save an estimated 2,000 lives each year.
99.8% of cervical cancer cases in the UK are preventable
Cancer Research UK
Symptoms of cervical cancer
Visit your GP if you experience any of the following symptoms:
- Unusual vaginal bleeding, including after the menopause, after sex, or between regular periods
- Changes to vaginal discharge
- Pain or discomfort during sex
- Unexplained pain in your lower back or pelvis
About cervical screening
During a cervical screening test (also called a smear test) a small sample of cells is taken from the cervix. Rather than testing for cancer itself, cervical screening tests for HPV, which may turn into cancer if left untreated. All eligible people automatically receive a letter from their GP inviting them to attend for screening.
Anyone with a cervix between ages 25 and 64 is eligible for cervical screening, which includes many trans men and/or non-binary people. Some trans men and/or non-binary people may have had gender confirmation surgery that involves removing the cervix, so will no longer be eligible. Trans women do not need cervical screening.
You will usually be invited for screening every five years between ages 25–64. After this age, screening will not routinely be offered.
Useful resources
Cervical screening (Macmillan)
Breast screening
About breast cancer
Breast cancer is cancer that starts in the breast tissue. It’s the most common cancer in the UK, affecting one in seven women during their lifetime. Most breast cancers (80%) occur in women over the age of 50; the older you are, the higher your risk. The earlier breast cancer is diagnosed, the better the chance of successful treatment, so it’s important to check your breasts regularly and to see your GP if you notice a change.
Men can also get breast cancer, but this is rare. Most men who get breast cancer are over 60. There’s no breast screening programme for men, so it’s important to be chest aware.
Breast screening programmes prevent around 1,300 women in the UK dying from breast cancer every year
Breast Cancer Now
Breast cancer symptoms
See your GP if you notice a change to your breast that’s new or unusual for you.
- A new lump or area of thickened tissue in either breast
- A change in the size or shape of one or both breasts
- A discharge of fluid from either of your nipples
- A lump or swelling in either of your armpits
- A change in the look or feel of your skin, such as puckering or dimpling, a rash or redness
- A rash (like eczema), crusting, scaly or itchy skin or redness on or around your nipple
- A nipple change, for example it has become pulled in (inverted)
About breast screening
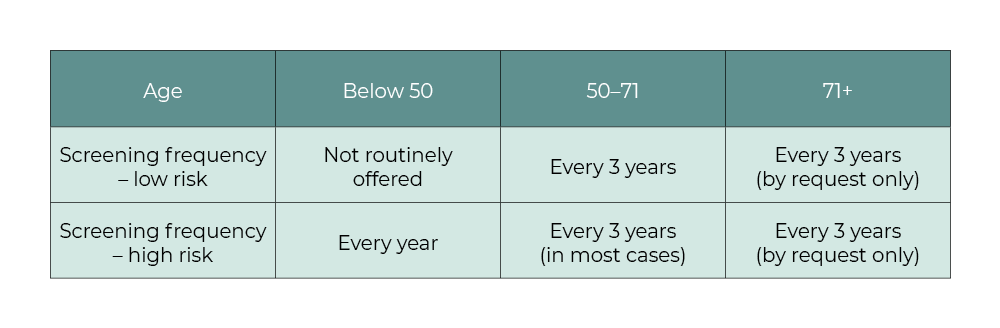
Breast screening uses a breast X-ray called a mammogram to look for cancers when they’re too small to see or feel. In the UK, women aged 50 to 71 are invited for a mammogram every three years as part of a national breast screening programme. Breast screening is more frequent, and begins at an earlier age, for women who have been assessed as having a moderate or high risk of developing breast cancer by a specialist in genetics or cancer.
The NHS breast screening programme offers screening to trans women, and also to trans men who have not had top surgery. However, you’ll only be automatically invited for screening if you are registered as a female with your GP.
The table below shows at what age and how often you might be invited for screening.
Useful resources
Benefits of breast screening (Macmillan)
Breast screening for women with a high risk of breast cancer
Bowel screening
About bowel cancer
Bowel cancer, often called colorectal cancer, affects the large bowel, which is made up of the colon and rectum. Most bowel cancers develop from pre-cancerous growths, called polyps, but not all polyps develop into cancer, and they can be removed early to prevent them becoming cancerous. Bowel cancer is the fourth most common cancer in the UK and the second biggest cause of cancer death. However, in the UK, bowel cancer survival has more than doubled in the last 40 years.
If diagnosed early, more than 90% of bowel cancer cases can be treated successfully
NHS
Symptoms of bowel cancer
Visit your GP if you experience any of the following symptoms:
- Bleeding from your bottom and/or blood in your poo
- A persistent and unexplained change in bowel habit
- Unexplained weight loss
- Extreme tiredness for no obvious reason
- Pain or a lump in your tummy
About bowel screening
As part of the NHS Bowel Cancer Screening Programme, eligible people are sent a home testing kit every two years to collect a small sample of poo to be checked for tiny amounts of blood which could be caused by cancer. Regular colonoscopies are recommended for people who have an increased risk of developing bowel cancer because of either their family history of the disease or genetic conditions they’ve inherited.
For most people the bowel screening programme will begin at 50 and you will be called every two years until you are 74. After this you won’t receive the routine appointments but you can request to continue with screening. These may be slightly different in the other nations of the UK. You can find out more here.
Useful Resources
Understanding bowel cancer screening (Macmillan)
While we have ensured that every article is medically reviewed and approved, information presented here is not intended to be a substitute for professional medical advice, diagnosis, or treatment. If you have any questions or concerns, please talk to one of our healthcare professionals or your primary healthcare team.
References
https://www.cancerresearchuk.org/
https://camdencarechoices.camden.gov.uk/